Wrist arthroscopy appeared in the 1970s, following the development of arthroscopy of more readily accessible joints. It was developed initially as a diagnostic tool, but because of the progress of other investigation tools such CT scan, artho-CT scan, and MRI, its diagnostic use subsequently decreased. In the past 15 years, wrist arthroscopy has become more of a treatment tool. Soon enough, it will become difficult to contemplate the treatment of wrist lesions without arthroscopy.
In 1972, Watanabe was the first to introduce an arthroscope in a wrist, following his initial work on knee arthroscopy published in 1969.
But is mainly Hempfling in Germany (1983) and Wipple in the US (1985) who really started to use wrist arthroscopy with a diagnostic purpose. During the late 1980s and the beginning of the 1990s, wrist arthroscopy developed throughout the world, mainly for the diagnosis of intra-articular lesions. Ostermann in the US, Pederzini in Italy, Bour and Saffar in France were the pioneers of this technique.
Since the 1990s, the true surgical arthroscopic techniques have considerably developed, with Luchetti in Italy, Doy in Japan, Geissler in the US, Lindau in Sweden, De Smet in Belgium, Ho in China, Stanley, Goddard and Yanni in England and Dumontier, Fontes and Mathoulin in France.
Equipment
This technique requires an expensive instrumentation. First, a traction system is required in order to distract the wrist. The patient lies supine, his arm fixed to the arm table, forearm and wrist in traction at 90°, with a 5 to 7 kg finger traction depending on the patient. An intermediate device is required in order to pull on the fingers, usually a Japanese finger trap. Video monitoring, a light source with optic fibres and a camera are also required, with an irrigation system using saline water.
The scope is very specific, with a 2.4 mm diameter and an oblique 30° lens connected to the light source. It is introduced in specific cannulas (3 mm diameter) which are connected to the irrigation system. Numerous surgical instruments are available : forceps, palpators, shavers and aspiration tools.
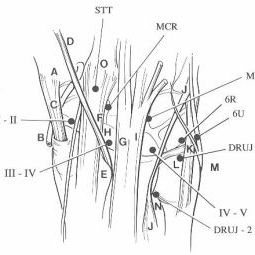
PortalsSeveral portals have been described, preserving the anatomy of the wrist so a to introduce the arthroscope and the instrument without injuring the surrounding anatomical structures.
- The radiocarpal joint is accessed through 4 main portals which are named according to the spaces dividing the different extensor compartments.
From radial to ulnar, the first portal 1-2 is located between extensor compartments 1 (abductor pollicis longus) and 2 (extensor carpi radialis tendons). This approach allows for visualization of the anterior aspect of the joint and is particularly useful for anterior ganglia.
The 3-4 portal is located between extensor compartments 3 (extensor pollicis longus) and 4 (extensor digitorum communis). This is the most classical portal of the radiocarpal joint, always performed first. It is located 1 cm distal to Lister’s tubercle. It allows for almost complete exploration of the whole radiocarpal joint, except for its anterior aspect.
The 4-5 portal is less utilized. It is located between extensor compartments 4 (extensor digitorum communis) and 5 (extensor digiti minimi).
Portal 6R is the second most common approach of the radiocarpal joint. It is located on the radial aspect of the 6th extensor compartment (extensor carpi ulnaris).
A further portal 6U, on the ulnar aspect of the extensor carpi ulnaris, had been described for irrigation. It is not often used because a specific portal for irrigation is not necessary in the wrist, and also because it is potentially harmful for the dorsal sensory branch of the ulnar nerve.
- At the level of the mediocarpal joint, there are 3 main portals. A radial medio carpal portal is located 1 cm distal to the radiocarpal 3-4 portal, allowing for exploration of most of the joint.
An ulnar mediocarpal portal is located at the junction between the hamatum, the lunate and the triquetrum. It is easily found thanks to a noticeable dip between the bones.
A third portal, called 1-2 mediocarpal or, more logically, STT (scapho trapezo trapezoidal), is nowadays more popular for surgical techniques related to the STT joint.
- There are three classical portals for the distal radioulnar joint. The distal radioulnar 1 portal, which is located 0.5 cm distal to the 6R radial carpal portal, allows for visualization of the distal aspect of the TFCC. A second portal, distal radioulnar 2, located 1 cm distal to the radiocarpal 4-5 portal, allows for visualization of the most proximal part of the distal radioulnar joint. Finally, a direct foveal portal allows for the treatment of some lesions of the TFCC.
Several rules must be adhered to in order to avoid complications. One should first inject a saline solution inside the radiocarpal and mediocarpal joints in order to distract them and facilitate access of the different tools without injuring the important anatomical structures. Skin incisions are performed horizontally to allow for better healing. For the same reasons, entry through the joint capsule is done with a curved smooth forceps. The cannula with a smooth trocart is introduced, then the trocart is replaced by the arthroscope.
A primary diagnostic assessment must be systematic, checking for all structures. There are a few “blind” zones at the level of the anterior and distal parts of the joint, and some palmar portals have been described. One first assesses the radiocarpal joint, and then the mediocarpal joint.
Between 1998 and 2011, we performed 2,000 wrist arthroscopy. All patients were treated with pneumatic tourniquet, as outpatients. Out of these 2,000 arthroscopies, only 42 (2%) were negative, i.e. without any diagnostic or therapeutic benefit. Of these 42 procedures, 34 were performed within the first 500 arthroscopies, as opposed to only 8 within the next 500 arthroscopies, showing an improvement in the choice of indications.
Indications can be organized in 7 groups:
- Assisted fracture treatments (distal articular radius and scaphoid: 7%)
- TFCC lesions (17%)
- Lesions of the intrinsic ligaments (scapholunate and lunotriquetral: 21%)
- Bone resections (radial styloidectomy, distal ulnar resection: 13%)
- Resection of ganglia (21%)
- Partial carpal prosthesis (2.5%)
- Other techniques (wrist arthrolysis, synovectomy: 14.5%)
Currently, the first two groups (assistance to the treatment of fractures and treatment of TFCC lesions) are considered indisputable indications which have refashioned the treatment of these lesions.
1 - Arthroscopically assisted treatment of fractures Articular fractures of the distal radiusDisplaced articular fractures of the distal radius require anatomic reduction. Many studies have shown that a remaining articular step greater than 2 mm produces joint arthritis at 5-year follow up in more than 90% of cases. In addition, ligament lesions are often associated. Wrist arthroscopy facilitates anatomic reduction of these articular fractures through direct visualization of the different fragments and allows for precise diagnosis and sometimes treatment of the associated intra articular lesions.
After the arthroscope has been introduced, the impacted fragments are reduced with a K wire or palpator introduced in the fracture site. Reduction and fixation of some small size, central fragments seem nowadays impossible without arthroscopic assistance.
Assistance for the treatment of scaphoid fracturesIn the past few years, many authors have advocated screw fixation of scaphoid fractures, which reduces immobilization time and seems to facilitate bone healing. For the past few years, we have been using a percutaneous screw fixation through a very limited anterior approach. The arthroscope enables to control the reduction through a medio carpal approach, while making sure that the head of the screw is not protruding in the joint at the level of the proximal pole thanks to the exploration of the radiocarpal joint. It is also possible to reduce displaced fractures with the use of a small instrument introduced through the mediocarpal 1-2 portal. When complying with these rules, results are often spectacular, allowing patients to use their wrist as early as the day following surgery.
2 - Arthroscopic treatment of TFCC lesionsThe triangular fibrocartilage is an important stabilizer of the distal radioulnar joint. Its treatment through an open approach has always been difficult. In our experience, it represents 17% of wrist arthroscopies. The majority of cases (92 cases) were ulnar tears of the ligament from its insertion on the ulnar styloid.
The presence of blood supply on the peripheral part of the TFCC allows for suture of the ligament. This type of lesion occurs mainly in sportsmen during forced supination movements with the wrist flexed, particularly in fencing, golf and tennis. The diagnosis is difficult, mostly clinical, sometimes confirmed by arthro-CT scan and MRI, knowing that there can be false negative and false positive images. Arthroscopy enables to perform a complete intra articular checking of the radiocarpal joint, with assessment in the ulnar area of the ligament tear and, at the same time, arthroscopic suture of the ligament.
The perforation is confirmed by a palpator, making sure not to confuse it with the normal styloid recess. The palpator enters easily underneath the TFCC, allowing for palpation of the ulnar head. Through the distal radioulnar 1 portal,, an intramuscular needle is introduced percutaneously through the articular capsule, obliquely directed distally and radially. Under arthroscopic control, one monitors its exit through the TFCC torn flap.
An absorbable suture is passed outside-in through the needle, then held with a forceps and retrieved through the 6R portal. A second intramuscular needle is introduced 0,5cm away from the first one, in a parallel to the first one, 0.5 cm away at the level of the TFCC. Another absorbable suture is passed through this second needle and retrieved through the 6R portal. The two sutures are tied together outside of the joint and the loop is reintroduced into the joint at the level of the distal radioulnar 1 portal. The reinsertion of the TFCC is check arthroscopically. Wrist distraction is then discontinued, the wrist is positioned in slight extension and ulnar deviation and a second knot is performed at the level of the distal radioulnar 1 portal. Wrist position in extension and ulnar deviation is then maintained for 6 weeks in a splint.
3 - Treatment of intrinsic ligament lesionsThey represent 21% of our cases. Together with TFCC lesions, they represent almost half of the indications of arthroscopic repair of wrist intrinsic ligaments.
The scapholunate ligament is most frequently involved.
4 - Bone resectionsBone resections represent 13% of our cases. These are mainly styloidectomies and distal resections of the ulna.
Radial styloidectomyRadial styloidectomy has been performed for various indications (sequelae of scapholunate tears, of distal radius fracture, of nonunion of the scaphoid proximal pole…). The arthroscope is introduced through a 3-4 portal, and the burr through a 1-2 portal. Styloidectomy is performed as needed under arthroscopic control until complete removal of the cartilage lesions. The postoperative course has always been extremely simple, with immediate mobilization. In two cases, we performed a styloidectomy in weight lifters who sustained styloid cartilage crush injury during their sport. In both cases, which were bilateral, surgery allowed the patients to return immediately to their sport without any pain.
Resection of the distal ulna in ulnolunate impingementUlnolunate impingements are most often secondary to distal radius fractures. The distal radioulnar index becomes positive (long ulna) because of the relative shortening of the radius, ultimately leading to hyperpressure between the ulnar head and the proximal aspect of the lunate. This hyperpressure rapidly creates an alteration of the carpal cartilage surfaces. When the ulnar variance is less than 5 mm, arthroscopic resection of the distal ulna is a simple and reliable technique.
The arthroscope is introduced through a 3-4 radiocarpal portal, allowing for joint exploration. A second 6R radiocarpal portal enables to treat potential lesions and the ulnolunate impingement.
Arthroscopy remains the best diagnostic tool to evaluate the severity of ulnolunate impingement. Indeed, it allows for direct visualization of cartilage wear. It is even more useful in early lesions, which can only be revealed by the arthroscope because they are limited to the area of hyperpressure between the ulna and the lunate. In case of positive ulnar variance inferior to 5 mm, surgical treatment of the lesion can also be performed arthroscopically. It consists in partial resection of the ulnar head under arthroscopic control, for which the postoperative course is relatively pain free. After exploring the joint, the most common finding is a central wear of the TFCC, with the ulnar head bulging in the radiocarpal joint. Articular assessment looks for and most often finds degenerative cartilage wear at the level of the ulnar head. At this stage, such chondropathy is not detectable on classical X-rays and rarely on CT-scans, due to the small size of the lesion. This cartilage lesion is responsible for pain. At this stage, partial resection of the distal ulna results in the disappearance of pain by suppression of the impingement. The arthroscope is introduced through a 3-4 radiocarpal portal, and a micro forceps with aspiration is introduced through a 6R radiocarpal portal. One first increases the size of the central tear of the TFCC, and then the resection of the bulging part of the ulna is performed arthroscopically with the help of a burr.
Peroperatively, passive movements in pronation and supination are required in order to perform a planar resection, from the anterior aspect all the way to the posterior aspect of the ulna head, while preserving the distal radioulnar joint. After water drainage, the small skin incisions are left open, the wrist is left free to move and the patient can immediately resume mobilization.
5 - Resection of wrist gangliaWrist ganglia are usually due to capsular anomaly. Dorsal ganglia result from degenerative lesions of the dorsal wrist capsule in the area of the scapholunate ligament. There are very often degenerative microcysts adjacent to the ganglia, embedded in the capsule, requiring resection of the adjacent joint capsule together with resection of the ganglia.
Ganglia of the anterior aspect of the wrist represent 20% of hand ganglia. They occur mostly between the flexor carpi radialis and abductor pollicis longus tendons. They originate usually from the radiocarpal joint but can be located away from their origin.
Many treatment options have been offered, from abstaining to open surgery. Surgical treatment is the most effective but can lead to many problems, such as unsightly scars, neuroma of the sensory branch of the radial nerve, or joint stiffness.
In addition, the proximity of the radial artery and nerve makes this surgery risky. Arthroscopic resection of dorsal and anterior wrist ganglia is our method of choice because of the uneventful postoperative course and because this technique prevents the majority of complications which have been described.
Resection of dorsal gangliaAll our patients have been operated under regional anesthesia and pneumatic tourniquet, as a outpatient procedure. The first step consists in locating the ganglion by drawing its contour. Then, thanks to a needle, one spots the proximal and distal boundaries of the ganglion. After inserting the arthroscope through the ulnar border of the joint thanks to the radiocarpal 6R portal and the ulnar midcarpal portal, we place an intramuscular needle at the level of the most proximal and most distal margins of the ganglion which enables us to outline precisely both the ganglion and the pathologic surrounding capsule. The pedicle of the ganglion is easily located inside the joint, most often facing the scapholunate ligament at the level of the midcarpal joint.
One then creates an approach directly through the ganglion. This approach is located slightly medially to the 3-4 radiocarpal and midcarpal portals. The mucus is then drained by means of external pressure. Then, under arthroscopic control, the ganglion, the synovitis and the joint capsule are resected with a shaver. The resection is about 1 to 2 cm2. The extensor tendons are perfectly visualized at the end of the procedure, and one must be careful not to injure them.
We do not close the skin incisions, thus allowing for water surplus drainage. Patients are discharged the same day without any immobilization of the hand and wrist, which they can use normally a soon as the anesthesia fades away. Resection of anterior ganglia
We use a 3-4 radiocarpal portal to insert the arthroscope. Anterior ganglia are mostly developed at the radiocarpal joint level.
The first operative step consists in identifying the origin of the ganglion. Through simple external pressure on the ganglion, one can clearly identify its origin, which is located between the radioscaphocapitate and radiolunotriquetral ligaments. One then creates a 1-2 radiocarpal portal. Using a shaver introduced through this lateral portal, one resects the pedicle of the ganglion and then the anterior capsule, which is often thin between the two ligaments. External pressure on the ganglion by the assistant facilitates the resection. As soon as an opening is made in the wall of the ganglion, mucus spreads out and disturbs arthroscopic vision. It is drained, then under arthroscopic control, the articular capsule, the synovitis and the ganglion are resected. Usually, the resection amounts to 1 cm2. At the end of the procedure, the flexor pollicis longus tendon is easily identified.
Arthroscopic resection therefore seems like a reliable and elegant solution.
6 - Arthroscopic wrist arthrolysisArthroscopic arthrolysis can be an alternative to open arthrolysis, the latter being susceptible to iatrogenic complications. However, this is a demanding technique which should be limited to surgeons with extensive experience with arthroscopy. After inserting the arthroscope in the radiocarpal joint through the 3-4 portal, a needle is inserted. This may prove difficult because of frequent degenerative modifications. It allows through a 4-5 or 6R portal to start shaving the ulnar part of the fibrosis. This is a difficult and slow procedure. As soon as intra articular vision improves, it is possible to treat the 3 important radiocarpal areas responsible for stiffness:
- A fibrous “wall” between the scapholunate ligament and the radial crest between the lunar and the scaphoid fossa.
- The dorsal “cul de sac” of the capsular joint, which is often totally obturated and adherent to the dorsal bone surface. One should resect all fibrosis and, if possible, part of the joint capsule.
- The anterior aspect of the joint capsule, for which one can take advantage of the 1-2 radiocarpal portal in order to resect the adhesions.
The procedure is completed by a systematic exploration of the midcarpal joint. Physiotherapy is initiated immediately after surgery. Anticipated results are often obtained quickly, and the number or rehabilitation sessions was limited.
7 - Insertion of partial wrist implantsThree main indications can be performed through wrist arthroscopy : replacement of the proximal pole of the scaphoid in non vascularised fragmented necrosis, implant interposition in scapho-trapezio-trapezoidal arthritis (STT), and carpometacarpal arthritis (CMC). Those are rare indications,representing only 2% of our cases. However, in carefully selected cases, these techniques, very simple for the patient, result in significant improvement of preoperative symptoms.
Treatment of nonunion and necrosis of the proximal pole of the scaphoid is difficult, with unpredictable results, especially in older people. Over time, they lead to radioscaphoid arthritis which progressively involves the whole wrist with carpal collapse.
The proximal pole of the scaphoid can be replaced by a specific implant adapted to the kinematics of the carpus. Thanks to this tridimensional reorientation during wrist movements, the implant remains stable throughout physiological movements, requiring no additional fixation with the scaphoid or periprosthetic encapsulation. The implant is made of pyrocarbon, a material which has already been proven to be totally biocompatible. Not subject to wear and chemically inert, the pyrocarbon implant generates no bone wear, which allows it to slide against the surrounding cartilage and ligaments so as to adopt the position of lesser resistance against the walls of its cage. Because it does not create any adhesions to its surrounding walls, it does not have any support to initiate a dislocation. Its modulus of elasticity is almost identical to that of the bone, therefore allowing for perfect tolerance. Its friction ratio is extremely low during friction against bone and cartilage.
During a first operative step, the arthroscope and its guide are inserted in the radiocarpal joint through a 4-5 radiocarpal portal. After identification of the proximal pole, one creates a second 3-4 radiocarpal portal. This portal should be slightly larger than usual, about 1.5cm, in order to facilitate removal of the proximal pole and insertion of the implant. The arthroscope can be easily inserted in this portal, allowing direct access to the nonunion area.
A radial midcarpal portal can be used to assess cartilage and control implant insertion.
Resection of the proximal pole is not always easy, depending on the age of the lesion. Occasionally, one encounters a small proximal pole which appears necrotic, at times multi-fragmented, and weakly attached to the lunate by a few ligament fibers. With small instruments such as little scissors, these attachments are sectioned under arthroscopic control. It is then easy to remove the proximal pole with a forceps.
A trial implant is then inserted in the radiocarpal joint in place of the proximal pole, and it is always satisfying to see how the implant positions itself properly. It is then replaced very easily by the permanent prosthesis, under arthroscopic control. The 3-4 radiocarpal joint is closed with a single suture. A protective dressing is applied for one week, and no splint is required. Mobilization is initiated immediately, allowing the patient to self-determine his range of motion depending on postoperative pain. If necessary, rehabilitation can be initiated after the third week.
Prosthetic replacement of the scaphoid proximal pole with a partial pyrocarbon implant through an arthroscopic technique can be a permanent as well as elegant solution in older patients with severe arthritic lesions. It can also represent a temporary yet effective and simple solution in younger patients who experience pain but have healthy cartilage around the necrotic lesions.
Other indicationsThis field is rather wide. Apart from wrist arthrolysis, which has become our standard, one can perform synovectomy, treatment of cartilage lesions, and everything that a surgeon’s skill and imagination will allow: sutures of capsular lesions, interposition in some cartilage lesions, partial arthrodesis, treatment of scaphoid nonunion, etc...
Wrist arthroscopy has progressively become a reliable technique which has improved our understanding of wrist anatomy and encouraged a less iatrogenic therapeutic approach. The therapeutic benefits of wrist arthroscopy have been largely demonstrated as many countries have reported reliable and reproducible case series. The quality of recovery in our patients, the growing number of indications, and the apparent accessibility of the procedure must not conceal the reality : wrist arthroscopy is a costly technique which does not allow for mediocrity. The learning curve is long and must be well supervised.
Wrist arthroscopy has an undeniable future and will most probably become mandatory for all surgeons who treat wrist joint lesions.

In 20 years of existence, the INSTITUT DE LA MAIN has become one of the main hand and upper limb surgery centers in Europe. Its nine surgeons on staff can treat all hand and upper limb problems.
Institut de la Main
Clinique Bizet
21 rue Georges Bizet
75016 PARIS
Front Desk : +331 84 13 04 56
Hand Emergencies : +331 84 131 131