The Brachial Plexus is a complex anatomical nerve structure connecting the spinal cord at the cervical level with the nerves supplying cutaneous and muscular innervation of the entire upper limb.
The plexus is formed by the ventral rami (roots) of the lower 4 cervical nerves (C5 C6 C7 C8) and the first thoracic nerve (T1).
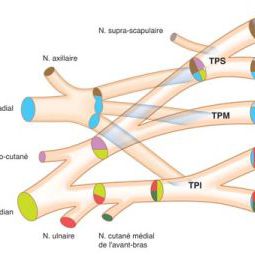
The roots connect themselves to form the trunks: C5 and C6 roots form the upper trunk, C7 forms the middle trunk while C8 and T1 roots form the lower trunk. Afterwards, each trunk divides into two branches: an anterior and a posterior one, which give origin to the cords (lateral, posterior and medial) that will distally contribute to form the nerves destined for the arm. The names anterior, posterior or medial define the relationship of the cords with the axillary artery.
It is interesting to situate topographically the different parts of the plexus in order to better understand the mechanisms of lesions and to facilitate the clinical examination and the diagnosis of the level of lesion.
Actually, the roots occupy the interscalene space, very close to the cervical spine. The trunks are situated in the supraclavicular region while their divisions forming the cords lie behind the clavicle; the cords (lateral, posterior and middle) occupy the infraclavicular region while the division into the distal nerves is completed in the axillary region.
There may be anatomical variations in the plexus mainly at the level of C7 division and in the formation of cords and distal nerves, which surgeons must be aware of, since it can influence the diagnosis of the level of lesion and consequently the strategy of repair.
Mechanisms of Injury Stretching injuries are the more frequent lesions of brachial plexus since motorcycle accidents are the main etiology in the majority of cases.
Usually, a violent shock of the head against the ground provokes a sudden and abnormal augmentation of the angle formed by the cervical spine and the shoulder. In this situation, the brachial plexus, more frequently at the level of the spinal foramina, is stretched and, depending on different factors, a variety of nerve lesions can occur.
The nerve lesions vary from a simple stretching without a real rupture to a complete avulsion of the roots from the spine. In the same plexus we can find an association of rupture and avulsion lesions at different root levels.
The retaining system of roots at the foramen is stretched to the point that its rupture leads to a direct stretching to the nerve root itself. When no retaining is present, the roots can be avulsed from the spine (see figure below).
In high velocity accidents, associated bone and vascular trauma may aggravate the nerve lesions.
Generally, the upper roots have stronger protective anatomical structure as compared to lower roots and this can explain, in total palsies, the quite constant avulsion of lower roots from the spine whilst upper roots are more frequently ruptured outside the spine.
Frequently, the impact of the upper limb with an obstacle can provoke severe bone lesions at the level of the shoulder, and the nerve lesions will be situated more distally from the spine, at the level of the cords. The association with scapula, clavicle, and humerus fractures is very frequent in these types of lesions. This leads to the possibility of a double level of nerve lesions that can complicate both the diagnosis and surgical treatment.
Less frequently, the plexus can be directly damaged by a cutting mechanism which is more likely provoked by a work-related accident or by voluntary infliction. In these cases, the nerve lesions will be less extensive even if the frequent association with vascular lesions (subclavian and/or axillary artery) can seriously aggravate the prognosis, rendering the surgical treatment more urgent.
When dealing with an acute traumatic lesion of the brachial plexus, the questions one must answer are the following:
Which part of the plexus has been damaged?
The answer to the first question is quite easy after a correct clinical examination. Even if in every root, the nerve fibres destined to the distal function are variably mixed, in a schematic way we can assess that:
After a correct clinical examination, one is generally able to assess the level of lesions as supraclavicular (root’s level), infraclavicular (cord level), or more distal (nerves).
We will classify the supraclavicular palsies as:
We will classify the infraclavicular palsies, i.e. lesions located under the clavicle, into lateral cord, posterior cord or medial cord lesions. In many occasions, as mentioned above, the lesions are combined retro and infraclavicular, with more cords involved and with possible double level of nerve damage.
The more frequently involved nerve lesions associated to root and/or cord lesions are: musculocutaneous, axillary, suprascapular and radial nerves.
Which is the level of root’s lesion?This is a crucial point in BP palsies sincethe possibility and the strategy of repair, and of course the quality of functional results we can obtain from the repair itself, depend on this assessment. The roots can be damaged outside the foramina (postganglionic or rupture lesions) or inside (preganglionic or avulsion lesions). The presence of root's stump will allow for nerve gap repair with grafts, while the absence of suitable stumps (avulsion) will require nerve transfer (neurotizations). The diagnosis of pre or postganglionic lesions could be clinical even if, as we will see, MRI will help in a substantial way in definition of the real level of lesion.
The upper roots are less frequently avulsed as compared to lower roots. This fact depends on anatomical conditions that allow a better defence from traction injuries of the upper roots while lower roots lack of this type of anatomical structures.
Clinical Examination
Clinical examination is of paramount importance since it can be an easy way to assess the extent of the lesion with a high degree of accuracy (number of roots involved and level of nerve lesions).
Examination of muscle function is the first fundamental step with special regards of proximally innervated muscles as Serratus muscle or Rhomboid muscles which can help to detect possible avulsion of the upper roots.
The presence of a Claude Bernard-Horner sign can lead to the diagnosis of a quite sure avulsion of lower roots.
Examination of sensation in the different territory of the arm is very important to help to determine the level of lesions.
Other clinical examinations include the study of the possible associated bone and joint lesions which can help from one side assessing the level of nerve lesions and from the other side allow to predict the limits of the possible functional recovery. For the same reasons, it is very important to evaluate the vascular conditions of the arm assessing the radial pulse, in absence of which an arteriogram or Doppler study are indicated. This will be useful in order to evaluate the condition of the muscles we are planning to reinnervate, and subsequently modify when necessary the strategy of repair. Moreover, knowing the anatomical conditions of the vessels (interruption of subclavian or axillary artery and presence of a collateral vascularisation) is of paramount importance for a safe reconstructive surgery.
Pain is another clinical sign to take into account. Quite constantly, root avulsions are associated with severe pain, mainly referred to the hand since the lower roots are mostly avulsed.
This pain is therefore an indirect sign of root avulsion and, since it may frequently reach unbearable levels for the patient, it needs to be treated as early as possible in specialized pain clinics.
Instrumental examination
X-rays are useful to detect sequelae of skeletal injuries that can interfere with plexus repair (callus on the clavicle) or to suggest a double level lesions (fracture of the scapula for suprascapular nerve, head of the humerus for axillary nerve and diaphysis of the humerus for radial nerve).
Fracture of transverse processes of the spine is normally associated with very proximal root lesions. A radiological study of diaphragm function is mandatory to detect possible lesions of phrenic nerve that can be associated with avulsion of C5 root.
The huge improvement in imaging given by 3D MRI allowed in the last years to detect with a high level of precision root avulsions. MyeloTAC still gives a good support in diagnosing preganglionic lesions.
Electrophysiological studies may give an important support in the diagnosis of the level of lesions but unfortunately even the evoked potential studies cannot precisely detect a preganglionic lesion that is the crucial point in brachial plexus lesions. Anyway EMG may be useful in the first months after injuries to eventually detect possible spontaneous recovery.
In presence of vascular lesions with lack of radial pulse, it is important to study the vascularization of the arm through Doppler exam or arteriograms, mainly to know the exact definition of the collateral vessel formation. This will be of paramount importance during the surgical dissection of the plexus in order to avoid reducing the vascular support to the arm.
Indications for Surgery
The main question is: what is the ideal time for surgery?
There is a general agreement that the time window for BP lesion repair must not exceed 6 months from injury, while different opinions exist about how early the repair of a brachial plexus lesion should be performed. There are few indications to operate in emergency, generally in association with vascular lesions; in these situations, it is quite impossible to assess the real level of traction injuries and consequently to perform a correct complete repair. Moreover, the longer operative time added to the emergency vascular repair may be dangerous in these kinds of patients; nevertheless the cooperation of the plexus surgeon with the vascular surgeon, whenever possible, may help to facilitate the vascular reconstruction, sparing in this way the nerve structures which will be repaired in better conditions in a second step. In the past, some surgeons suggested operating traumatic plexus traction injuries within the first week with the purpose of avoiding fibrotic scar tissue. The advantage is real from the technical point of view, nevertheless, we think that the risks are really higher than benefits. The only exceptions are the rare sharp wounds of the brachial plexus, since there is the possibility to repair the nerves immediately with direct sutures.
In all the other cases, we consider that the ideal time for surgery is between the 2nd and the 3rd month from injury; this would be sufficient to allow for stabilization of the associated lesions and the general condition of the patient, and to better assess the possible spontaneous recovery.
Due to the frequent complex associated lesions (skeletal, cutaneous,vascular etc), it is advisable to wait for the stabilization of general conditions of the patient before surgical repair.
We consider that the period between the second and third months from the trauma is the ideal time for surgical repair of the brachial plexus. The age of the patient is not considered as a real limitation for surgery anymore since we have experienced functional recovery even in patients over sixty y.o.
In conclusion, when facing a brachial plexus lesion once the diagnosis has been correctly assessed, we suggest waiting as long as necessary to solve the associated lesions. Meanwhile, an early rehabilitation program should be started whenever possible.
Delayed and late Surgery
Very few reports in literature regard the late repair of nerve lesions and of brachial plexus in particular. There is a general consensus to define as late a surgery performed at least one year after the trauma. The presence of fibrillation detected with an EMG study is considered a prerequisite to attempt a late repair of the plexus. Even if there are many evidences of possible recovery of single muscles, generally biceps or supraspinatus, through neurotizations (nerve transfers) after 2 years from the trauma, the results are still unpredictable; this fact renders late surgery a rescue repair which may be attempted in some case if not widely suggestible.
A proper treatment of brachial plexus injuries needs multiple and different competences possibly coordinated by the same person/s
For these reasons, we suggest, when dealing with brachial plexus lesion:
Surgical repair
The type of surgical repair will depend on the type and extension of lesions. In presence of a sharp wound of the plexus either very proximal (root’s level) or more distal (cord’s level) the repair will be easily done by a neurorrhaphy.
In presence of postganglionic lesions, that is rupture of the roots in which either proximal and distal portion of the ruptured nerve are present, the gold standard of repair is to re establish the continuity of the nerve by means of nerve grafts.
This repair will be more or less complete depending on the number of roots stump available to be repaired. The problems start with the very frequent association of root avulsion that means no proximal stumps available to allow an anatomical reconstruction of the nerve gap with grafts.
This repair will be more or less complete depending on the number of roots stump available to be repaired. The problems start with the very frequent association of root avulsion that means no proximal stumps available to allow an anatomical reconstruction of the nerve gap with grafts. In these situations the only option is to try to repair the distal part of a nerve which lacks its proximal connection by means of neurotizations.
Neurotization can be defined as a nerve transfer or nerve by pass in order to bring nerve sources out of the plexus to re-innervate distal stumps no more connected with the proximal ones.
If in a multiple root avulsion lesions we can find at least one or two root’s stump the grafts will be distributed from the remaining roots to the entire distal part of the plexus. This will be defined as an intraplexual neurotization. Examples of extraplexual neurotization are spinal accessory nerve sutured to suprascapular nerve in avulsion of upper roots or intercostals nerves sutured to musculocutaneous nerve in total palsies or contralateral healthy C7 root used to bring re-innervation to the avulsed roots.
Since to perform a neurotization one must intentionally section a healthy nerve, one must carefully evaluate the cost-benefit in order to concentrate on a unique target nerve or a portion of it avoiding to provoke a substantial loss of function at the donor site.
It is obvious that neurotization offers a limited repair and thus, especially in extended palsies, must be multiple (accessory nerve, intercostals nerves, contralateral C7 etc).
Strategy of Repair
Upper palsies C5 C6 –C5 C6 C7C5 C6
The C5 C6 lesion is very common. The roots can be ruptures or avulsed. There are cases where one root is avulsed and the other ruptured.
ONLY EXPLORATION OF THE ROOTS CAN GIVE AN EXACT VIEW OF THE SITUATION
The preferable way of repair is grafting between the good stump and the distal trunks. It implies a precise assessment of the quality of the stumps, sometimes using chemical staining, often, with experience, by clinical examination. Only grafting can give a recovery of the whole muscle groups innervated by the upper roots
Neurotizations can be very useful when the roots are avulsed or when they have a poor quality. The most common neurotizations are:
There are other, less common, neurotizations using Intercostal or Pectoralis nerves.
Strategy
If there are 2 usable roots:
C5 C6 C7
The association of a C7 lesion makes the repair much more difficult in case of avulsion, as the ulnar nerve and the Triceps may be involved.
Strategy
If 3 roots are ruptures:
It is not possible to repair all the functions by nerve surgery. Some neurotizations are possible in the arm (intercostal) or in the forearm (FCR, pronator) but it will be necessary to add some secondary tendon transfers (especially in the wrist).
Complete brachial plexus injuryWhen all roots and especially the lower (C8 T1) roots are injured, it is called complete brachial plexus.
In most cases, unfortunately, the lower roots are avulsed from the spinal. They have no chance of spontaneous recovery.
Up to now, the treatment of complete brachial plexus has been limited to repair by grafts or neurotizations of the upper plexus in order to recover movements in the shoulder and elbow. Apart from the rare case where the lower roots were ruptured and could be repaired, the attempts of reinnervation of the hand muscles by grafts, or neurotizations by intercostal nerves have given very poor results and in most cases, the hand has been abandoned.
A new perspective has been operated by the chinese authors, using the contro-lateral C7 root. Although the CC7 transfer with graft has not changed dramatically the prognosis, its use with a direct coaptation to the lower has proven in many cases very effective (WANG).
We are now using this technique either alone or combining it with other techniques when possible.
Strategy:
1 - Complete palsy with C5 C6 or C7 intact:
The donor site is the C7 root on the opposite site. The root is cut as distally as possible and passed posterior to the oesophagus and anterior to the vertebra.
On the injured side, the Lower Trunk (C8 and T1) is mobilized from the arm to the foramen allowing, if possible, a direct suture with the opposite C7 root. The direct suture is very important for the quality of recovery and if a few centimetres are missing, it is preferable to shorten the humerus in order to allow a suture without tension rather than to use a graft. The consequences of harvesting the C7 root are limited : paresthesias in the thumb and index, weakness of the Triceps or Finger extensors. These anomalies usually disappear after a few months. There may be initially some difficulties to use the recovered hand by moving the opposite arm but after some learning, the control is good.
Results in Complete Paralysis
The repair of complete paralysis has always been a challenge.
For more than 40 years, attempts of repair of the lower trunk have never given consistent results. The classical repairs with grafts and local neurotizations (intercostals) do not lead to a regular recovery of the hand.
In our experience of 630 complete paralyses operated, only 20% had a five-roots avulsion. These are, of course, the most difficult cases.
From these cases, 200 had an attempt to repair the lower trunk, usually through grafts from the upper roots. Only 22% had some fingers flexion. The repair of the lower roots has such a bad reputation that many surgeons prefer to use all the good uppers roots available to repair the shoulder and elbow and abandon the hand, in the hope of some further surgery later (muscle transfers).
The occurrence of the contralateral C7 transfer has raised hopes to improve those results. However, the results of CLC7 transfer by classical means (subcutaneous graft) have not proven to largely modify the results. Bathia has recently shown that this technique gave him approximately 40% of positive results : a non decisive improvement. Tu, using vascularized nerve graft obtained 65% recovery of the hand.
The great breakthrough came when Wang improved the technique, using the pre-spinal root and with a direct suture at all costs between C7 and the lower trunk (even when needed, shortening of the humerus). He systematically added a neurotization of the posterior trunk by the phrenic nerve. Not only 72% of the patients have wrist flexion, 64% fingers flexion, but they have recovery of a good overall use of the arm. We visited the patients and were impressed by their results.
This is why, since beginning of 2013, we have started to use the procedure, as long as the patient is willing and accept the potential drawbacks
Results in upper palsy
In upper palsy ( C5-C6 and C5-C6-C7), the results are good. With grafts, our results of C5-C6 reconstruction show 66% of good results in the shoulder, 78% of good results in Elbow flexion.
Avulsion injuries of C5-C6 used to be very difficult to repair with poor results. Since the use of neurotizations, the results have been widely improved: with neurotizations, our results are 80% of good results in the shoulder and 90% of good elbow flexion.
When a sufficient period of time from nerve repair (or lack of repair) without a useful functional recovery has elapsed, a secondary surgery strategy can be advised. We can define as secondary surgery all these operations devoted to restore, even if partially, some fundamental functions not achieved by nerve repair or spontaneous recovery; this can be obtained by tendon or muscle transfers by means of changing their original insertion in order to obtain new movements by a different motors.
Secondary surgery, even called palliative surgery, must be considered as a forced limited solution for a deficit whose original cause can’t be restored. The ideal time to perform this surgery will depend on the functional territory of the arm whose function we intend to restore. For the shoulder, for instance, whose nerves need at least two years to lead to a functional recovery, we will indicate a secondary surgery not before 2 years. For more distal functions to be restored, for instance for wrist extension we will wait at least three to four years that is the time that a nerve regeneration will need to reach the distal target so far from the point of lesion/repair.
The reason why the results we can obtain by secondary surgery in plexus palsies are very frequently only partial, is that the motors which can be used to substitute the deficits are very limited and moreover quite always not sufficiently strong. In fact a prerequisite for this type of reconstructive surgery apart avoid to add functional impairment to the arm, is to use sufficiently strong muscles which is rarely the case in sequelae of plexus palsies.
Just to give some examples for abduction of the shoulder a trapezius muscle can be reinserted more distally from his original scapular insertion to reach the humerus, changing in this way his physiological lever arm in order to recover a certain degree of abduction. For elbow flexion, depending on the motors at our disposal, we can transpose the epitroclear muscles, latissimus dorsi or pectoralis major to substitute biceps function.
To restore wrist extension, transfer of wrist flexors are usually used. In absence of any muscles to be transposed there is the possibility to completely transplant a muscles, usually the gracilis muscle harvested from the thigh, that will be revascularized and reinnervated by microsurgical techniques. We must underline that this sophisticated and complex surgery can partially restore only one single function and even If repeated will never succeed to obtain a useful result in terms of function of the hand.
After secondary surgery and a period of 6 to 7 weeks of immobilization of the arm necessary to favour the anatomical healing of the transfer, a long period of rehabilitation will be needed. Physiotherapy will aim at reinforcing the muscles in their new anatomical site in order to recover a reasonable function and to allow the patient to learn the new cortical schema of recovering movement.

In 20 years of existence, the INSTITUT DE LA MAIN has become one of the main hand and upper limb surgery centers in Europe. Its nine surgeons on staff can treat all hand and upper limb problems.
Institut de la Main
Clinique Bizet
21 rue Georges Bizet
75016 PARIS
Front Desk : +331 84 13 04 56
Hand Emergencies : +331 84 131 131